Insulin is a hormone that is produced by the pancreas and plays a crucial role in regulating blood glucose levels in the body. Insulin signals the body’s cells to take up glucose from the bloodstream and use it for energy or store it as glycogen or fat. Blood sugar level regulation is very important for our health and is very complex.
Insulin affects the body in several ways. First, it helps regulate blood glucose levels by facilitating the uptake of glucose into cells. Second, insulin promotes the synthesis of glycogen in the liver and muscles, which helps to store excess glucose for later use. Finally, insulin also promotes the synthesis of fatty acids in adipose tissue, which helps to store excess glucose as fat.
Let’s explore the following questions:
- What is insulin and insulin resistance?
- What is blood sugar level and how is it measured?
- Why do our bodies need to regulate blood sugar levels?
- What happens when our blood sugar level is too low or too high?
- How to control blood sugar level regulation and have optimal insulin resistance?
- What problems arise from insulin resistance?
- What factors outside of diet affect blood sugar level regulation and insulin resistance
- Sleep
- Exercise
- Environmental factors
- Stress
- Diabetes as a result of chronic high blood sugar levels.
- From healthy to diabetic – the stages of insulin resistance.
- Diabetes, life expectancy, and Healthspan
- Summary
Insulin and insulin resistance
Insulin is a hormone produced by the pancreas that helps regulate blood sugar levels. Glucose is a type of sugar that is the body’s primary source of energy. After eating, glucose from food enters the bloodstream, and insulin is released to help transport the glucose into cells where it can be used as energy.
Insulin resistance occurs when cells in the body can no longer respond to insulin as effectively as they should. This means that more insulin is needed to move glucose from the bloodstream into cells, and the pancreas may eventually become unable to produce enough insulin to keep up with the demand.
This can occur when the body is regularly exposed to high levels of glucose, such as when a person eats a diet high in foods with a high glycemic index (GI). High GI foods are quickly absorbed and cause a rapid spike in blood sugar levels.
What is blood sugar level (blood glucose level) and how is it measured?
The blood sugar metric, also known as blood glucose level, measures the amount of glucose, a type of sugar, in the bloodstream at a given time. Glucose is an important source of energy for the body’s cells, and the blood sugar level is tightly regulated by the hormone insulin, which is produced by the pancreas.
Insulin is responsible for transporting glucose from the bloodstream into the body’s cells, where it can be used for energy or stored for later use. When blood glucose levels are high, such as after a meal, insulin levels rise to facilitate the transport of glucose into the cells. When blood glucose levels are low, such as during fasting or exercise, insulin levels decrease, allowing stored glucose to be released from the liver and other tissues.
Insulin resistance occurs when the body’s cells become less responsive to insulin, and as a result, blood glucose levels remain elevated. Over time, this can lead to chronically high blood glucose levels, which can damage the body’s tissues and organs and increase the risk of various health problems, such as type 2 diabetes, heart disease, and stroke.
How to measure blood sugar levels?
Measuring blood glucose levels is an important diagnostic tool for detecting insulin resistance and other metabolic disorders. Fasting blood glucose levels are typically measured after an overnight fast and can provide information about an individual’s overall blood glucose control. Hemoglobin A1c (HbA1c) is another blood test that measures average blood glucose levels over the past 2-3 months and is commonly used to monitor blood glucose control in people with diabetes.
Blood glucose levels are tightly regulated by insulin, and the measurement of blood glucose levels can provide important information about insulin resistance and overall blood glucose control. Regular monitoring of blood glucose levels is important for maintaining good health and preventing complications associated with insulin resistance and diabetes.
The normal range for blood sugar levels in a healthy adult is between 70 and 99 mg/dL (milligrams per deciliter) when measured after fasting (not having anything to eat or drink except water for at least 8 hours). After eating, blood sugar levels will typically rise and then fall back down to the normal range.
Blood sugar levels can be measured using a device called a glucometer, which is a small, portable device that uses a drop of blood from a finger prick to measure the glucose level in the blood. The test is usually done by pricking the finger with a lancet, which is a small, spring-loaded needle, to obtain a drop of blood. The blood is then placed on a test strip and inserted into the glucometer, which will then give a reading of the blood sugar level.

Another method to measure blood sugar level is through a blood test called Hemoglobin A1C, which gives an average of blood glucose levels over the past 2-3 months. This test can be done by taking a blood sample from a vein and it is typically done in a laboratory.
The normal range for blood sugar levels may vary depending on the individual and whether they have diabetes or other medical conditions. Your healthcare provider can give you more information on what the normal range is for you and how often you should test your blood sugar levels.
Why do our bodies need to regulate blood sugar levels?
Our bodies need to regulate blood sugar levels because glucose is the primary source of energy for our cells. However, if blood sugar levels get too high or too low, it can cause serious health problems.
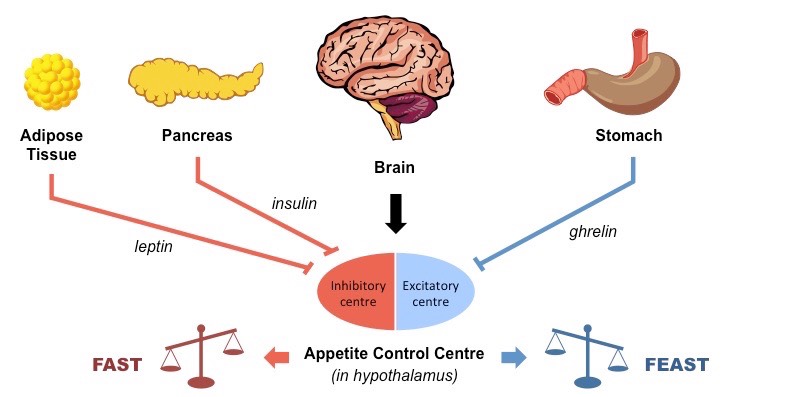
The body regulates blood sugar levels through a complex process that involves several hormones, including insulin and glucagon. Insulin is produced by the pancreas and helps to move glucose from the bloodstream into cells where it can be used as energy. Glucagon, also produced by the pancreas, works in opposition to insulin, signaling the liver to release stored glucose into the bloodstream when blood sugar levels are too low.
The body also regulates blood sugar levels through the use of glucose transporters, which are responsible for moving glucose into cells. The body can also increase or decrease the number of glucose transporters depending on the body’s needs.
Our bodies can also regulate blood sugar levels through the use of feedback mechanisms. For example, when blood sugar levels are high, the body will release insulin to lower them, and when blood sugar levels are low, the body will release glucagon to raise them.
The human body has several mechanisms in place to regulate blood sugar levels and ensure that they remain within a healthy range. When these mechanisms are not working properly, it can lead to conditions such as diabetes and hyperglycemia.
Why is low blood sugar dangerous?
When the blood sugar level drops below normal levels you can feel the effects. Low blood sugar, also known as hypoglycemia, is dangerous because it can cause a range of symptoms that can affect the brain and the body’s ability to function properly. When blood sugar levels drop too low, the brain does not have enough glucose to function properly, which can cause confusion, difficulty concentrating, and even seizures or loss of consciousness in severe cases.
What is a low blood sugar level?
Low blood sugar is called hypoglycemia. A blood sugar level below 70 mg/dL (3.9 mmol/L) is low and can harm you. A blood sugar level below 54 mg/dL (3.0 mmol/L) is a cause for immediate action.
When blood sugar levels drop too low, the body will release the hormone glucagon which signals the liver to release stored glucose into the bloodstream. However, if the blood sugar levels are too low and the body can’t release enough glucose, the brain may not have enough energy to function properly, which can lead to symptoms such as:
- Shakiness and tremors
- Sweating
- Hunger
- Headaches
- Dizziness
- Irritability
- Fatigue
- Confusion
- Difficulty concentrating
- Seizures or loss of consciousness (in severe cases)
If low blood sugar is not treated promptly, it can lead to serious complications such as coma or even death. People with diabetes are at higher risk for low blood sugar because of the medications they take to lower blood sugar, but anyone can develop low blood sugar if they skip a meal, exercise too much, or drink alcohol. It is important to recognize the signs of low blood sugar and to have a plan in place for how to treat it.
Why is high blood sugar level dangerous?
Spikes in blood sugar can be dangerous because they can damage blood vessels and organs over time. When blood sugar levels rise quickly, the body produces more insulin to try to bring them back down. However, when this happens repeatedly, the cells in the body can become resistant to the effects of insulin, which can lead to insulin resistance.
What is a high blood sugar level?
For the majority of healthy individuals, normal blood sugar levels are as follows:
Between: 4.0 to 5.4 mmol/L (72 to 99 mg/dL) when fasting
Up to: 7.8 mmol/L (140 mg/dL) 2 hours after eating
For people with diabetes, blood sugar level targets are as follows:
Before meals: 4 to 7 mmol/L for people with type 1 or type 2 diabetes
After meals: under 9 mmol/L for people with type 1 diabetes and under 8.5mmol/L for people with type 2 diabetes
How does a high blood sugar level damage cells?
High blood sugar levels can cause damage to cells because glucose is a form of sugar that can damage proteins and other molecules in the body when present in high concentrations. One of the ways it does this is through a process called glycation, which occurs when glucose molecules bind to proteins or lipids in the body, forming new molecules called advanced glycation end products (AGEs).
AGEs can damage cells in several ways. For example, they can cause inflammation, which can lead to damage in blood vessels and other organs over time. AGEs can also damage the proteins in the body, including enzymes, which can affect the way cells function.
In addition, high blood sugar levels can also cause damage to cells by making them more vulnerable to damage from other sources, such as free radicals. Free radicals are molecules that can damage cells and contribute to the development of chronic diseases such as diabetes and cancer.
When damaged cells are no longer functioning as they should and when they are poorly defended from outside threats, this can lead to a knock-on effect on other cells. A cascade of failure is possible.
Excessive glucose can also overwork the pancreas, which leads to the overproduction of insulin. This can cause the pancreas to eventually become unable to produce enough insulin to keep up with the demand, leading to insulin resistance and type 2 diabetes.
High blood sugar levels can cause damage to cells by a variety of different mechanisms, including inflammation, protein damage, and damage from free radicals. It is important to maintain healthy blood sugar levels to avoid this kind of damage.
What problems arise due to insulin resistance?
When insulin resistance is present, glucose remains in the bloodstream instead of being taken up by the cells, leading to high blood sugar levels (hyperglycemia). Over time, high blood sugar levels can cause damage to the blood vessels, leading to an increased risk of cardiovascular disease, kidney damage, nerve damage and eye problems. Insulin resistance also contributes to the development of type 2 diabetes, which is characterized by persistently high blood sugar levels.
Problems that may occur as a result of insulin resistance include an increased risk of type 2 diabetes, high blood pressure, heart disease, and obesity. Long-term insulin resistance can also increase the risk of developing other health problems such as polycystic ovary syndrome (PCOS) and nonalcoholic fatty liver disease (NAFLD).
High-glycemic diet and its dangers
A high glycemic diet is one that is high in foods that cause a rapid and large increase in blood sugar levels. These foods have a high glycemic index (GI) rating, which measures how quickly a food raises blood sugar levels compared to glucose (a reference food with a GI of 100). High glycemic foods include processed foods and refined carbohydrates, such as white bread, sugary drinks, desserts, and other sweeteners.
Eating a high glycemic diet can lead to chronic high blood glucose levels and eventually diabetes because these foods cause rapid spikes in blood sugar levels, which can overwhelm the body’s ability to produce and use insulin, leading to insulin resistance and eventually, diabetes.
Signs that a diet is too high on the glycemic index include:
- Consistently high blood sugar levels
- Constant hunger and cravings
- Fatigue and low energy levels
- Mood swings
- Difficulty losing weight
- Increased risk of heart disease
- Increased risk of diabetes
It’s worth noting that a diet high in glycemic index foods is not the only cause of diabetes, however, it can be a contributing factor to the development of diabetes, especially when combined with other risk factors such as obesity, physical inactivity, and family history of diabetes.
How to keep insulin resistance at bay and blood sugar at an optimal level?
Keeping blood sugar levels and insulin resistance at optimal levels can be achieved through a combination of diet, exercise, and lifestyle changes. Some ways to achieve this include:
- Eating a healthy diet: A diet that is low in processed foods, added sugars, and saturated fats, and high in fiber, fruits, vegetables, whole grains, and lean protein can help keep blood sugar levels within a healthy range. Eating smaller, more frequent meals throughout the day can also help keep blood sugar levels stable. However, intermittent fasting can also help by maintaining blood sugar levels low.
- Getting regular exercise: Regular exercise can help improve insulin sensitivity and lower blood sugar levels. Aim for at least 30 minutes of moderate-intensity exercise, such as brisk walking or cycling, most days of the week.
- Maintaining a healthy weight: Being overweight or obese can contribute to insulin resistance, so maintaining a healthy weight can help improve insulin sensitivity and lower blood sugar levels.
- Getting enough sleep: Sleep is important for overall health and well-being. Not getting enough sleep can affect insulin sensitivity and blood sugar levels, so aim for 7-9 hours of quality sleep per night.
- Managing stress: Chronic stress can affect insulin sensitivity and blood sugar levels, so it’s important to find ways to manage stress, such as through exercise, meditation, or therapy.
- Avoiding smoking and excessive alcohol consumption: smoking and excessive alcohol consumption can increase the risk of diabetes and other health problems.
- Monitoring blood sugar levels regularly: Monitoring blood sugar levels regularly using a glucometer can help you understand how certain foods and activities affect your blood sugar levels and make adjustments accordingly.
It is also important to note that environmental factors such as pollution and exposure to certain chemicals can also affect our bodies ability to keep blood sugar levels within an optimal range. This is why it is important to be aware of the environmental factors that may affect your health and take steps to minimize your exposure to them.
Overall, maintaining a healthy lifestyle by eating a balanced diet, getting regular exercise, maintaining a healthy weight, getting enough sleep, managing stress, and avoiding smoking and excessive alcohol consumption can help keep blood sugar levels and insulin resistance at optimal levels.
How does long-term fasting, intermittent fasting, or a time-restricted eating pattern improve blood sugar regulation and improve insulin resistance?
Intermittent fasting, or time-restricted eating patterns, has become popular recently and among the benefits, it provides for health is its effect on body blood sugar regulation.
Intermittent fasting can affect blood sugar levels and insulin resistance in several ways. Intermittent fasting is an eating pattern in which individuals alternate periods of eating with periods of fasting.
One of the main effects of intermittent fasting on blood sugar levels is that it can help lower blood sugar levels and improve insulin sensitivity. This is because when the body is in a fasted state when you’re hungry, it must rely on stored glucose (glycogen) and fat for energy, which can lead to a reduction in blood sugar levels.
When losing weight it means that cells, due to fasting are low on energy and they absorb glucose available from the bloodstream. Blood sugar level drops and after the glucose is consumed, fat is converted and used for energy. This is called a metabolic switch. The metabolic switch is when the body’s preferential shift from the utilization of glucose from glycogenolysis to fatty acids and fatty acid-derived ketones.
Intermittent fasting can also help improve insulin sensitivity, which is the ability of cells to respond to insulin. This is because, during fasting, insulin levels drop, which can help make cells more sensitive to insulin. This means that when insulin is present, it is more effective at moving glucose from the bloodstream into cells, which can help lower blood sugar levels.
Additionally, Intermittent fasting can also have a positive effect on weight loss, which can also help improve insulin sensitivity. This is because when you lose weight, your body becomes more sensitive to insulin and is better able to use it to move glucose into cells.
There are several types of intermittent fasting such as the 16/8 method, where individuals fast for 16 hours and eat during an 8-hour window, or the 5:2 method, where individuals eat normally for 5 days and restrict calorie intake to 500-600 calories for 2 non-consecutive days.
Intermittent fasting may not be suitable for everyone, especially for people with diabetes, and pregnant or breastfeeding women. It’s recommended to speak with a healthcare professional before starting an intermittent fasting regimen and to monitor blood sugar levels regularly to ensure that they remain within a healthy range.
Sleep and blood sugar level regulation and insulin resistance
Sleep plays an important role in our health and has a profound effect on how our body deals with nutrients. Adequate sleep helps regulate blood sugar levels and insulin resistance. Lack of sleep or poor sleep quality can affect the body’s ability to regulate blood sugar levels and insulin sensitivity.
Sleep deprivation can affect the body’s ability to produce and respond to insulin, which can lead to an increase in blood sugar levels. This is because when the body is sleep deprived, it produces more stress hormones such as cortisol, which can make cells less sensitive to insulin and make it harder for the body to regulate blood sugar levels.
Poor sleep quality can also affect glucose metabolism, which is the way the body uses glucose for energy. Studies have shown that people who have poor sleep quality tend to have higher levels of glucose in their blood, which can contribute to the development of diabetes and other health problems.
Inadequate sleep can also affect the hunger hormone ghrelin, making people eat more and therefore, leading to weight gain which is a major risk factor for type 2 diabetes.
In contrast, getting enough quality sleep can improve insulin sensitivity and help regulate blood sugar levels. Adequate sleep can help reduce inflammation and improve the way the body uses insulin, which can help lower blood sugar levels.
It is recommended to aim for 7-9 hours of quality sleep per night and to maintain a consistent sleep schedule. Avoiding stimulating activities before bed such as using electronic devices and consuming caffeine, and creating a relaxing bedtime routine can also help improve the quality of sleep.
It’s important to speak with a healthcare professional if you have concerns about how sleep may be affecting your blood sugar levels or insulin resistance.
Exercise Effect on blood sugar level regulation and insulin resistance
Exercise is the best thing you can do for your body after getting adequate sleep. It is a pillar of human health and it is irreplaceable in helping our bodies function properly. One of the ways exercise can be instrumental in making the most of our diet is by regulating blood sugar levels and improving insulin sensitivity. Regular exercise can make the process even smoother.
Exercise can have a positive effect on blood sugar levels by helping to lower them and improve insulin sensitivity. When you exercise, your muscles use glucose for energy, which can help lower blood sugar levels. Exercise can also increase the number of glucose transporters in the cell membranes, making it easier for cells to take up glucose from the bloodstream.
During exercise, muscles also absorb more glucose from the bloodstream, therefore, reducing the levels of glucose in the blood. This is why blood sugar levels often decrease after exercise.
Exercise can also increase the body’s sensitivity to insulin, which is the hormone that helps move glucose from the bloodstream into cells. When insulin sensitivity is improved, less insulin is required to move glucose into cells, which can help lower blood sugar levels.
It’s also important to note that the type, intensity, and duration of exercise can affect blood sugar levels differently. Aerobic exercises such as brisk walking, cycling, swimming, and jogging, are known to have a stronger effect on blood sugar levels than resistance training.
It is recommended to consult a healthcare professional before starting an exercise program if you have diabetes or other medical conditions. Also, it’s important to monitor blood sugar levels before and after exercise, to ensure that they remain within a healthy range and adjust the exercise plan accordingly.
Diabetes as a result of chronic high blood sugar
Diabetes is a chronic condition characterized by high levels of sugar (glucose) in the blood. There are two main types of diabetes: Type 1 and Type 2. Type 1 diabetes is an autoimmune disorder in which the body does not produce enough insulin, a hormone that regulates blood sugar levels. Type 2 diabetes is a metabolic disorder in which the body does not properly use insulin.
Diabetes takes a while to develop but it is a serious health risk. Usually, there are steps that the body experiences before it becomes full-blown diabetes. As long as your pancreas can make enough insulin to overcome your cells’ weak response to insulin, your blood sugar levels will stay in a healthy range. If your cells become too resistant to insulin, it leads to elevated blood glucose levels (hyperglycemia), which, over time, leads to prediabetes and Type 2 diabetes.
From being healthy to diabetes as a result of chronic insulin resistance
Becoming diabetic does not happen overnight, it takes time to develop.
- Healthy: In this stage, the body’s cells respond properly to insulin, and the pancreas produces the right amount of insulin to regulate blood sugar levels.
- Insulin resistance: In this stage, the body’s cells begin to lose their sensitivity to insulin, and the pancreas produces more insulin to try to overcome this resistance. Blood sugar levels may begin to rise, but they are not yet high enough to be considered prediabetes or diabetes.
- Prediabetes: In this stage, blood sugar levels are higher than normal but not yet high enough to be considered diabetes. People with prediabetes are at an increased risk of developing type 2 diabetes and other health problems.
- Diabetes: In this stage, blood sugar levels are consistently high, and the body is not able to properly regulate them. This can lead to a range of health complications if left untreated, such as heart disease, kidney damage, and nerve damage.
It’s worth noting that not everyone will go through these stages in a linear fashion. Some people may develop diabetes without ever having prediabetes, while others may never progress beyond insulin resistance.
Diabetes can have a significant impact on both human longevity and healthspan. People with diabetes are at an increased risk of developing a range of health complications, such as heart disease, kidney damage, and nerve damage. These complications can lead to a decreased lifespan and a lower quality of life. Additionally, uncontrolled diabetes can also increase the risk of other diseases like stroke, blindness, and amputations.
Diabetes, life expectancy, and healthspan
At age 50 and beyond, life expectancy- the number of years a person is expected to live is 6 years shorter for people with type 2 diabetes than for people without it. Life expectancy can be increased by 3 years or in some cases as much as 10 years with interventions and medications.
Managing diabetes through lifestyle changes, such as eating a healthy diet, engaging in regular physical activity, and maintaining a healthy weight, can help to reduce the risk of complications and improve both longevity and healthspan. Medications, such as insulin and oral diabetes drugs, can also be used to help control blood sugar levels.
In summary, diabetes is a chronic condition characterized by high blood sugar levels, and it can have a significant impact on both longevity and healthspan. It can be managed through lifestyle changes and medications, but it’s important to be vigilant about monitoring and managing the condition to avoid complications.
Summary
Diet is a major contributing factor to insulin sensitivity.
There are ways to monitor blood sugar levels.
Lifestyle has a massive impact on insulin resistance and besides diet, sleep and exercise help to maintain balance.
Smoking and other harmful habits increase the risk of becoming diabetic.
There are a few stages between being healthy and becoming diabetic so there are warning signs.
Look after your health and learn about self-discipline and setting goals.